50F with fever and knee joint pains
50 year old female, health care worker ( aayamma in orthopedic hospital ) resident of miryalguda presented with complaints of fever since 1 week, nausea and vomitings for 3 days, Rt shoulder pain since 1 week.
She works in a orthopaedic hospital, does washing of patients clothes, OT gowns, other clothes with cleaning the hospital premises when ever it’s necessary. After reaching home she manages to do her work and take rest.
In 2005 when her parents went to daily work ( daily waged labourers ) met with an road accident and expired, following which in there memory she tattooed there names on her right forearm. ( similar tattoos where present on her both knees, couldn’t give exact reason for them ).
Since 10-11 year she had both knee joint pains for which she took analgesics with a frequency of 4-5 per month which did not effected her daily routine. Her son got married 10 years back, with daughter in law entering into her family, she got some rest and continues to work in hospital.
Since 1 year her knee joint pains has increased and worsened 4-5 months back with difficulty in walking. She reached an orthopaedician and received a shot of intra articular injection ( presumably steroids ) following which she get some relief and managed to do her work.
Since 4 months she had low grade fever, intermittent, episode lasting for 7-14 days with complete normalcy in between the episodes and associated with progressive worsening of knee pains. Since February 28th till date ( 2 1/2 months = 70 days ) she had 4-5 hospital visits which reveals persistent tachycardia, lower blood pressure ( SBP 80-90 mmhg ), documented elevation of inflammatory markers ( ESR, CRP ) 1 month back. Received Antibiotic cocktail ( piptaz, doxy, clindamycin, magnet forte ) in last 1 month.
On 18 th April she went to local physician in miryalguda and admitted, where her examination revealed tachycardia with HR 135 at normal body temp and blood pressure of 80/60 mmhg. Normal hemogram, Renal and liver functions. She was tested negative for widal ( titers < 1:80 ), Dengue, malaria and HIV serology.ECG showing sinus tachycardia with S1Q3T3. In view of further work up of pulmonary embolism / myocarditis she was referred to higher centre next day morning.
In Nalgonda work up for Pulmonary Embolism ( here after referred as PE ) was done with echo showing Normal sized chambers with No RWMA and Good LV systolic function. D dimers was slightly elevated with an rough value around 1100 IU/dl ( normal < 250-400). USG abdomen - normal study except renal calculi. In view of elevated D dimer and clinical distress ( tachypnea and spO2 94-95 on RA) CTPA was done which shows Negative study for PE. Patient denied further work up and get got symptomatic treatment and returned to her home. She was symptomatically improving and started to go to work after 5-6 days.
10 days back she had attended a marriage where she ate mutton curry following next day she had fever initially low grade, progressed to high grade with in 2 days associated with 3-5 episodes of vomitings, which was initially non bilious with last episode of bilious vomiting with food particles as contents and no blood. She reported generalised weakness and loss appetite with decreased meal consumption, she used to chew tobacco regularly since yrs which was stopped after this fever episode. She revealed appearance of oral ulcers and throat pain coinciding with fever. She also briefed about her right shoulder pain which was insidious in onset rapidly progressed over 3-4 days with difficulty and pain during movements around the joint which hampered her activities of daily living.
Quick examination revealed :
A patch of low density hair
Mild Conjunctival suffusions
Red Beefy tongue with curdy white precipitate on tongue ( poor oral hygiene / ?oral candidiasis )
Prominent neck swelling ( soft, no nodules) which moves with deglutition
Painless hyperpigmented lesions on palms
Distorted foot nails
Disproportionate tachycardia ( temp 100, HR 140 )
Pedal oedema
No JVP
Visceral fat
Easy bruising after removal of ecg leads
No organomegaly
Normal lung auscultation
Cardiac auscultation - occasional S3 with No murmurs
Painful restriction of abduction ( managed to initiated but restricted from 30 degree ) & internal rotation.
Mild Tender points present
Sensory ataxia with loss of joint proprioception
Mild slurred speech according to son and daughter in law
Labs :
Near normal CBP ( with available parameters in case sheet )
Normal renal functions
Mildly elevated liver enzymes ( mild elevation above UNL @ 54 iu/dl )
Hypoalbuminemia ( total proteins 5.6 and albumin 2.9 ) with urine dipstick albumin of + on CUE
Otherwise unremarkable CUE
Problem representation :
Elderly female - post menopausal status with no co-morbidities presented with chronic systemic inflammatory response syndrome (with B symptoms - malaise, loss of appetite, weight loss of over 6-7 kgs in last one month ) with acute exacerbation following an acute febrile illness, vomitings and new onset mono-arthritis of right shoulder with neck pains and peripheral neuropathy
Infections - TB, Hepatitis, Gram negative organisms, covid 19 & other health care associated bugs,
Autoimmune - thyroiditis, polymyositis
Malignancy - less likely - no localising symptoms
Toxins - nicotine
Endocrine - thyrotoxicosis, pheochromocytoma ( less likely )
Advised : Blood cultures, Thyroid function and coagulation studies with 24h UPCR.
Patient centered learning through pajr discussion
[5/13, 4:11 PM] Dr Rakesh Biswas Sir Hod Gm Kam: She denied this history in the afternoon rounds maintaining that her bilateral knee arthritis is just from a year!
[5/13, 4:24 PM] Dr Rakesh Biswas Sir Hod Gm Kam: Quick summary from today's afternoon bedside rounds :
PUO
Assymetric oligoarthritis
Hepatitis mild
Monocytosis
Myocarditis (resting tachycardia)
Waldeyer's ring involvement
Differentials :
Chronic viral? Chikungunya? (epidemiologically common in Telangana)
Other infections like mtb
Immune : Lupus, Sarcoid,
lymphoma
[5/13, 4:30 PM] saicharankulkarni: Okay sir will confirm this again.. she reported this history yesterday evening in front her son, daughter in law and @govardini.
[5/13, 4:36 PM] Dr Rakesh Biswas Sir Hod Gm Kam: @Dr govardhini reddy Jnr Gm Kam was presenttoday as well along with the son and daughter in law
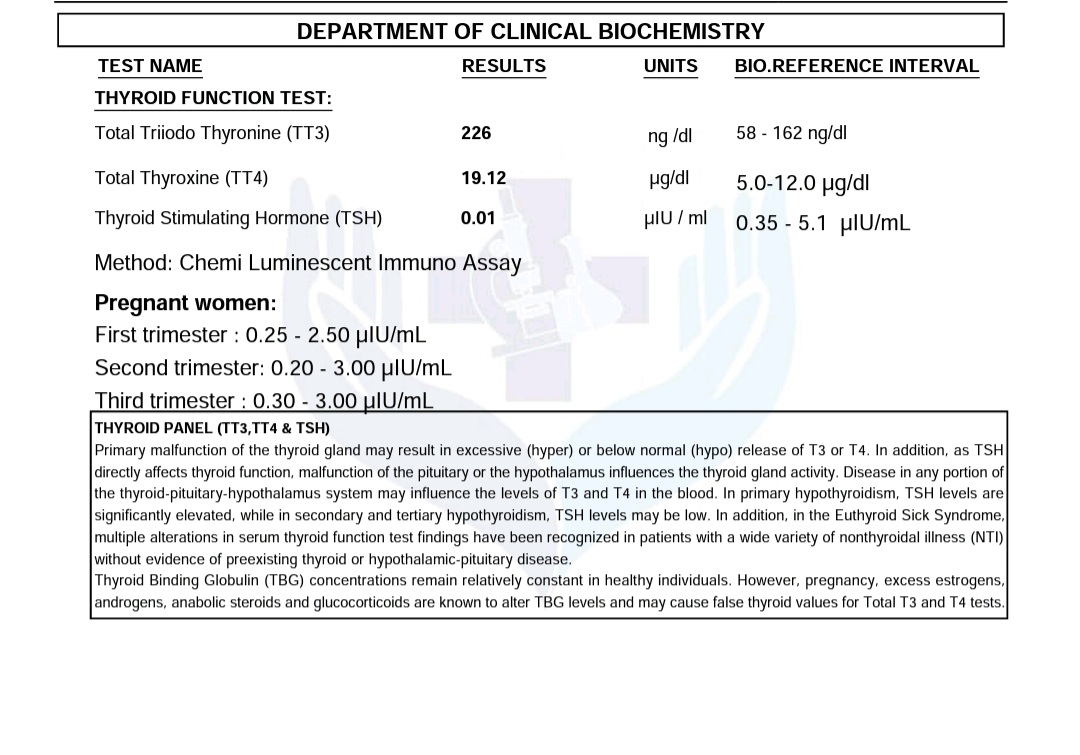
[5/13, 4:39 PM] saicharankulkarni: Hyperthyroidism was also on the list sir. Though she didnt report any heat intolerance but weight loss, fever, tachycardia.
@Dr govardhini reddy Jnr Gm Kam please share her thyroid report
[5/13, 5:21 PM] saicharankulkarni: @Dr. Dinesh Datta Jr Kam will there be any processing error if sample stored for 2 days..??
how to address her tachycardia..?
With increasing beta blocker dose to 50mg OD / BD..?
Will troponin helps to support our myocarditis theory..?
Any surrogate test for suspected hyperthyroidism ( apart from sending outside lab )
@Dr govardhini reddy Jnr Gm Kam @Dr. Dinesh Datta Jr Kam @Dr Keerthi Jnr Gm Kam @Dr. Venkat Sai👨🏼⚕ Jnr Kam
[5/13, 6:38 PM] Dr Rakesh Biswas Sir Hod Gm Kam: Send outside
Repeat daily EcGs and share here to look for changes
Review the literature on tachycardia in myocarditis and heart failure and share asap
[5/13, 6:46 PM] saicharankulkarni: The most common ECG abnormalities seen in myocarditis are:
Sinus tachycardia
Non-specific ST segment and T waves changes
Other ECG changes are variable, and may include:
Prolonged QRS
QT prolongation
Diffuse T wave inversion
Ventricular arrhythmias
AV conduction defects
With inflammation of the adjacent pericardium,
ECG features of pericarditis can also been seen (= myopericarditis)
[5/14, 4:41 PM] saicharankulkarni: Good 👏👏👏
Did we started her on any antithyroid drugs..??
@Dr. Venkat Sai👨🏼⚕ Jnr Kam did we increased her beta blocker dose to 50 mg..?
Thyroid storm is a clinical diagnosis for patients with pre‐existing hyperthyroidism. In determining whether or not a patient has thyroid storm the main systems to concentrate on are the CNS (ranging from being agitated to seizure), thermoregulatory system (rise in temperature), cardiovascular system (ranging from tachycardia to atrial fibrillation and congestive cardiac failure [CCF]), and gastrointestinal–hepatic system (ranging from nausea to vomiting and jaundice).
[5/14, 5:47 PM] Dr Rakesh Biswas Sir Hod Gm Kam: Switch to tablet propranolol 30 mg 8 hourly
Tablet carbimazole 40 mg stat and 10mg tid from tomorrow
@~Arefin Sadat and @~Manogyna the recent trend of fast track publications in cureus can be impactful as in this one here 👇
that offers good comisseration for our current inpatient here?
[5/14, 5:50 PM] saicharankulkarni: She is receiving Metoprolol sincr admission sir. Changed to propranolol after report.
[5/14, 5:52 PM] Dr Rakesh Biswas Sir Hod Gm Kam: What dose?
[5/14, 5:53 PM] saicharankulkarni: Temp - 100-100.9 - 10 points
Lethargy with excess sleepiness - 20
Nause and vomiting - 10
Tachycardia HR more than 140 - 25
Total of 65 sir.
[5/14, 5:54 PM] saicharankulkarni: She was reciving metaprolol 25 mg sir.
Replaced with propranolol 40mg Bd.
[5/14, 5:54 PM] saicharankulkarni: Metaprolol teesesi propranalol pettuko
[5/14, 5:54 PM] saicharankulkarni: Starr with 40 mg bD
[5/14, 5:55 PM] saicharankulkarni: In text with @Dr. Venkat Sai👨🏼⚕ Jnr Kam
[5/14, 6:03 PM] Dr. Venkat Sai👨🏼⚕ Jnr Kam: ok sir
[5/14, 6:10 PM] +91 88850 66656: Yes sir
I went through charan sirs blog on the patient and this publication perfectly aligns to review the literature that might be necessary in this patient’s case,like preference of propranolol keeping in view of her Thyroid status and history of persistent tachycardia.
[5/14, 6:50 PM] Dr Rakesh Biswas Sir Hod Gm Kam: Lethargy with excessive sleepiness was documented before admission? Post admission it would compete and conflict with the on duty staff?
[5/14, 7:13 PM] Dr govardhini reddy Jnr Gm Kam: She became lethargic and sleepy since the day of onset of fever 1 week back and she is saying that she never felt this way before or in previous episode of fever 1 month back sir
[5/14, 9:18 PM] Dr govardhini reddy Jnr Gm Kam: Sir
Tab.Carbimazole 40 mg stat dose and tab. propranolol 40 mg is given








Comments
Post a Comment