Bimonthly assessment jan.
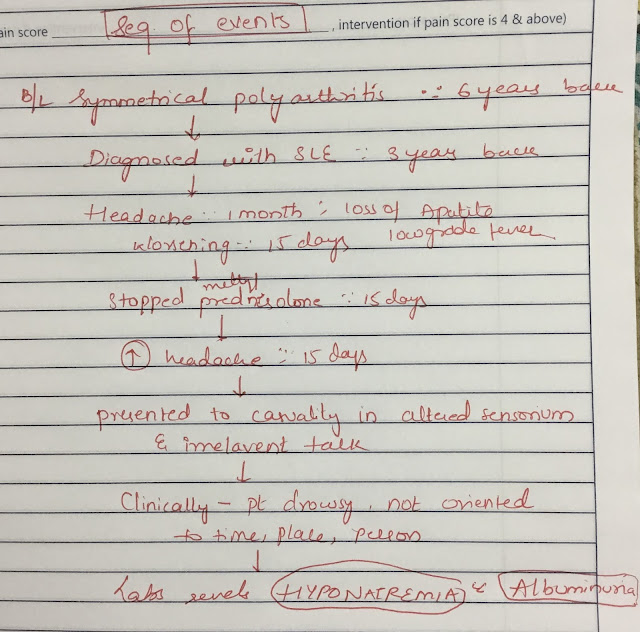
1) 26 year old woman with complaints of altered sensorium somce 1 day,headache since 8 days,fever and vomitings since 4 days.
Problem representation:
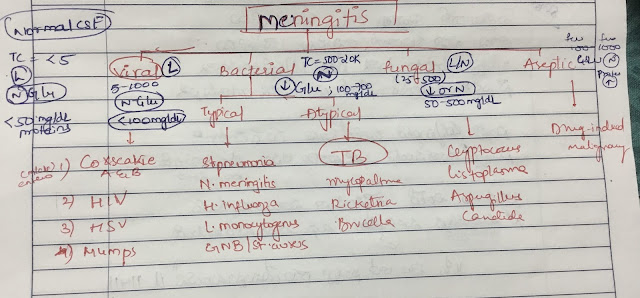
26 year old Immunocompromised lady presents with Acute onset Altered sensorium and signs of meningism.
Anatomical localisation:
In the background of immunocompromised State , length and tempo of the presentation I would think acute aetiology like infections, drugs and toxins.
With three years history of systematic lupus erythematosis where she was on methylprednisolone since three years leading to immuno suppression may flare up chances of infection. With detailed history the drugs which she was using like hydroxychloroquine , sulphasalazine,methylprednisolone, alandronic acid and gabapentin doesn’t explain her symptoms and on further probing the attenders at any point they refuse that she take poison or toxins
On the background of immuno suppression which symptoms like chronic headache fever neck pain loss of appetite Iwould think of infection which is involving her central nervous system likely result in altered sensorium and irrelevant talk.
On clinical examination Brudzinski and kernicks were negative though she had terminal neck rigidity and pain. Fever chart seems to be stepladder suggestive of enteric fever which is unlikely in this case as there are no features suggestive of enteric fever like pain abdomen vomitings loose tools etc
Considering the epidemiology i would list my differentials as tubercular meningitis, enteric fever, CNS lupus.
Rare possibility that non-steroidal anti-inflammatory drugs like ibuprofen can cause meningitis in patients with lupus. The most plausible explanation for the association is a hypersensitivity reaction involving the meninges. https://pmj.bmj.com/content/75/890/771

c) What is the efficacy of each of the drugs listed in her prior treatment plan that she was following since last two years before she stopped it two weeks back?
Hydroxychloroquine : Both HCQ and Pl were well tolerated in the 48-week trial. There were no remissions. With the exception of the patient assessment of joint pain, all other joint measures were similar between the groups. Twenty-nine patients withdrew before the end of the trial although only 2 patients withdrew for adverse drug effects.
https://pubmed.ncbi.nlm.nih.gov/7983646/https://pubmed.ncbi.nlm.nih.gov/7983646/
Bisphosohonates for steroid induce osteoporosis :
We included a total of 27 RCTs with 3075 participants in the review. Pooled analysis for incident vertebral fractures included 12 trials (1343 participants) with high‐certainty evidence and low risk of bias. In this analysis 46/597 (or 77 per 1000) people experienced new vertebral fractures in the control group compared with 31/746 (or 44 per 1000; range 27 to 70) in the bisphosphonate group; relative improvement of 43% (9% to 65% better) with bisphosphonates; absolute increased benefit of 2% fewer people sustaining fractures with bisphosphonates (5% fewer to 1% more); number needed to treat for an additional beneficial outcome (NNTB) was 31 (20 to 145) meaning that approximately 31 people would need to be treated with bisphosphonates to prevent new vertebral fractures in one person.There was high‐certainty evidence that bisphosphonates are beneficial in reducing the risk of vertebral fractures with data extending to 24 months of use. There was low‐certainty evidence that bisphosphonates may make little or no difference in preventing nonvertebral fractures.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6461188/
Oral corticosteroids:
Forty-one patients (21 randomized to prednisone and 20 randomized to placebo) experienced a serologic flare. Analysis of severe flares occurring <or=90 days from randomization revealed that 6 occurred in patients taking placebo and none occurred in patients taking prednisone (P = 0.007). Severe flares resulted in an increase in the prednisone dosage to >40 mg/day and/or the addition of an immunosuppressive agent. Furthermore, improvement in scores on the Systemic Lupus Erythematosus Disease Activity Index, decreased levels of anti-dsDNA antibodies, and increased levels of C4 occurred 1 month after initiation of prednisone treatment.
https://pubmed.ncbi.nlm.nih.gov/17075807/
Sulphasalazine:
I couldn’t find good literature regarding efficacy of sulphasalazine in SLE.
d) Please share any reports around similar patients with SLE and TB meningitis?
cases of bacterial meningitis without initial CSF pleocytosis in adults have rarely been reported. Only 26 cases, including the present case, were found in a search of English abstracts in the MEDLINE database. Patients with documented neutropenia were excluded (Table 1) (6–20). Of these, 11 cases had Streptococcus pneumoniae, 10 had N meningitidis, two had Escherichia coli, one had Proteus mirabilis, one had Listeria monocytogenes and one had Haemophilus influenzae. Blood culture was performed in 24 cases and bacteremia was detected in 19. The outcome was documented in 20 cases. Seven patients died and two exhibited auditory disorders. The timing of antimicrobial therapy was analyzed in 18 patients. Empirical treatment had not been implemented in five patients. Neutropenia is known to be associated with no response in CSF (11). Lukes et al (21) reported that 45% of neutropenic patients with bacterial central nervous system infection did not have pleocytosis. Fishbein et al (8) also reported two other patients with neutropenia caused by bacterial meningitis with normal CSF cell counts. Therefore, we excluded patients with neutropenia from the literature review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4211346/
e) What is the sensitivity and specificity of ANA in the diagnosis of SLE?
Of 1010 ANA test results reviewed, 153 were positive. The group with positive ANA test results included more patients aged 65 years or older than the group with negative ANA test results (30% vs 15%, P < .003). The diagnosis of systemic lupus erythematosus (SLE) was established in 17 patients, all of whom had positive ANA test results. Other rheumatic diseases were found in an additional 22 patients. The estimated sensitivity and specificity of the ANA test for SLE were 100% and 86%, respectively. For other rheumatic diseases, sensitivity and specificity were 42% and 85%, respectively. The positive predictive value of the ANA test was 11% for SLE and 11% for other rheumatic diseases. Specificity and positive predictive value for ANA testing in the elderly patients were lower than among younger patients.The sensitivity of the ANA test for SLE was high, but overall the positive predictive value was low for SLE or other rheumatic diseases. Sensitivity was low for ANA testing among patients with non-SLE rheumatic disease. More selective test ordering might improve the clinical utility of this test. Clinicians ordering the ANA test should be aware of the test's low-positive predictive value in settings with a low prevalence of rheumatic disease, particularly among older patients.
https://pubmed.ncbi.nlm.nih.gov/8678710/
2) Please go through the two thesis presentations below and answer the questions below by also discussing them with



Comments
Post a Comment