30M with post renal transplantation recipient status.
CBBLE UDHC SIMILAR CASES
Case of 29 year old male
February 05, 2021
30M post Renal transplantation recipient
FAMILY HISTORY:
He was 3 yrs old when in 1992 his paternal grandfather expired due to stroke.. His paternal grand mother also died due to stroke.. His elder aunt’s death was dramatically heralded when she vomited on the weaving machine and collapsed which presumably was due to vascular pathology mostly brain. In1990 father had a headche for which he went to an RMP and found to have elevated BP which he neglected and took symptomatic medication untill 2000 when he fainted while attending work.he was started on medication but eventually gave up for magneto therapy which he presumed to be better than medication.Father’s sister while cleaning the backyard fell unconsciousand died which was also presumed to be due to a vascular pathology.
One day in 2007 *SUDDENLY* his father noticed he had lost vision in one of his eyes, he was taken to a physician and found to have a BP of 230/110.. He was restarted on medication. In a weeks time father vision recovered which again hints out at a transient vascular pathology... In 2017 father had a chest pain and managed medically by a cardiologist for coronary artery disease. The same yr he had gone to a hospital in bangalore and found to have renal failure and was started on dialysis.The pt cousin sister expired at very young age due to complications of CKD and Anemia diagnosed very late. The maternal grandfather is still alive but was diagnosed with TB in middle age and apparently treated
PATIENT HISTORY:
2016 pt had visited a dentist for his tooth ache and found to have a BP of170/130.. After 2 months still his BP was the same after which he was adviced telmisartan 40mg.In the mean time he was receiving unknown medication for his ringworm infection.
In Dec 2018 pt experienced headache and vomitings went to a hospital adviced admission and given IV anti htns as he had an alarming BP valueof 240/130..He was discharged the next day after BP came down to170/90. sr creat found to be 3.5 was adviced amlodipine and torsemide.may 2019 when pt started experiencing headache pain abdomen blood stained vomitings SOB pt taken to hospital and creat found to be 6.15 and HB 6.0 he was adviced dialysis and blood transfusion. august 2019 when pt experienced SOB and chest pain. He was taken to a PG hospital in Kolkata where he was admitted in Pulmonology for his SOB.. 15 days he was evaluated and came to know it was his renal problem that had to be solved first and was discharged and sent to nephro opd.Theyarrived at kims on 16th sept.On presentation in opd we saw thin built poorly nourished young male with evident pallor..
On examination:
BP-150/90,PR-110,RR-26
Inspection: a visible apical impulse
Palpation: unequal chest expansion
Percussion: dull note in rt MA AA IMA IAA ISA
Auscultation: decreased breath sounds in rt MA AA IMA IAA ISA
BLOOD TRANFUSIONS DONE
TRATMENT:
16/9/2020:
Pleural tap done showed exudative picture with lymphocytic pleocytosis.. he had dialysis i/v/o his increased urea and creat and just when we had put the central IJV line on rt side he started to bleed..Bleeding was thought to be due to platelet dysfunction in uremia hence we carried out a dialysis by placing a Rt femoral central line and 1 SDP transfusion. bleeding stopped after a stitch. Pt wasstarted on anti htn.
TAB.Nifedipine 5mg QID to 10mg TID
INJ.LASIX
TAB.CLONIDINE
18th sep-Added INJ.CEFTAZIDIME,
INJ.AMIKACIN
(As klebsiella sp was isolated)
19th Oct -?Catheter Catheter induced sepsis Added INJ.CETRIAXZONE for 5days(Tlc- 26000 came down to 8000)
2nd Nov - pericardial rub
4th Nov- initiation of ATT
7th Nov- added PRAZOSIN
10th Nov- added TELMI 40mg
11nov -spironolactone to NTG and labetolol iv infusion
13th Nov- onset of pulmonary edema and hypoxia and got intubated
14th Nov- ICD placed
15th Nov- extubated and ATT stopped
After brainstorming for the cause behind flash pulmonary edema and reviewing literature,a conclusive decision was made that Rifampicin, as a potent ezyme inducer, was causing failure of anti-htn medication thus ATT stopped.
21st Nov- ATT reinitiated with
T.ETHAMBUTOL
T.PYRAZINAMIDE
T.LEVOFLOXACIN
FROM JAN TO MARCH2020
T.NICARDIA 10MG QID
T.TELMA AM 40/5 H/S
T.LASIX 20MG TID
T.ALDACTONE 25MGOD
T.PRAZOSIN 2.5MG TID
T.OROFER XT LATER INJ.ERYTHROPOIETIN 2000IU/SC
ONTUESDAY,THURSDAY ,SATURDAYS:
T.LABETOLOL 100MG TID
T.PYRAZINAMIDE 1500MGOD
T.ETHAMBUTOL 1000MG OD
T.LEVOFLOX 500MG OD
ALTERNATE DAY HEMODIALYSIS
Advice at Discharge:
T.NICARDIA 10MG QID
T.TELMA AM 40/5 H/S
T.LASIX 20MG TID
T.ALDACTONE 25MGOD
T.PRAZOSIN 2.5MG TID
T.OROFER XT
ON TUESDAY,THURSDAY,SATURDAYS:
T.LABETOLOL 100MG TID
T.PYRAZINAMIDE 1500MG OD
T.ETHAMBUTOL 1000MGOD
T.LEVOFLOX 500MG OD
Follow Up REVIEW TO GENERAL MEDICINE OPD AFTER FITNESS
X Ray
29 M WITH SEVERE HYPERTENSION, RENAL FAILURE, FUO, LARGE PLEURAL EFFUSION, HFpEF AND INTERMITTENT PULMONARY EDEMA
CONSIDERED FOR RENAL TRANSPLANT
Patient came to Our institute for renal transplantation in February 2021 after all
Date of Operation
16-4-21LIVE RENAL TRANSPLANTATION ( RECIPIENT)
Diagnosis
CKD STAGE- 5 ON MAINTAINENCE HAEMO DIALYSIS
Breif Case History and Clinical Findings
K/C/O CKD STAGE 5 ON MAINTAINENCE HAEMODIALYSIS WITH RESISTANT HTN CAME TO HOSPITAL FOR LIVE RENAL TRANSPLANTATION ( RECIPIENT ) EMPIRICAL TREATMENT FOR TB (ATT FOR 4 MONTHS ) 2019
K/C/O HTN + NOT A K/C/O DM , BA , EPILEPSY
PATIENT CAME TO HOSPITAL WITH SERUM CREATININE- 37.0 UREA - 240 PATIENT STARTED ON MHD AFTER CONFORMING ESRD -5 PRE OPERATIVE EVALUATION PULMONOLOGIST REFERRAL DONE I/V/O RECURRENT PLEURAL EFFUSIONS ON PREVIOUS ADMISSIONS(SEPT 2019)WHICH WERE LOCULATED FOR WHICH ICD WAS ALSO PLACED . PATIENT WAS STARTED ON ATT ON 4TH NOVEMBER AND STOPPED ON 15TH NOVEMBER 2019 I/V/O RESISTANT HYPERTENSION AND PULMONARY EDEMA.RIFAMPICIN WAS STOPPED AS IT WAS POTENT ENZYME INDUCER AND CAUSING FAILURE OF ANTI HTN MEDICATION . 21ST NOVEMBER 2019, PATIENT WAS STARTED ON ATT WITH T.ETHAMBUTOL AND T.PYRAZINAMIDE AND TAB.LEVOFLOXACIN WHICH HE USED FOR 6 MONTHS.
PULMONOLOGIST HAD GIVEN FITNESS TO TAKE UP FOR SURGERY UNDER GENERAL ANAESTHEISA WITH MILD RISK
GASTRO ENTEROLOGIST REFERAL DONE I/V/O FITNESS FOR SURGERY AND HAD GIVEN FITNESS FOR SURGERY
CARDIOLOGIST REFERAL DONE I/V/O FITNESS FOR SURGERY CARDIOLOGIST HAD GIVEN FITNESS TO TAKE UP FOR SURGERY UNDER GENERAL ANAESTHEISA WITH HIGH RISK.
Investigation
HRCT OF THORAX PLAIN :
SEGMENTAL ATELECTASIS IN RIGHT LUNG MIDDLE LOBE WITH MILD FIBROSIS - SEQUALAE OF OLD INFECTION MINIMAL RIGHT PLEURAL EFFUSION HYPERDENSE LIVER >85-90 HU - D/D DRUG INDUCED/METABOLIC CAUSES/ - TO RULE OUT HEMOCHROMATOSIS /IRON OVERLOAD /STORAGE DISORDERS B/L SMALL SIZED KIDNEYS CONSISTENT WITH CKD CORADS 1
USG DOPPLER OF PELVIC VESSELS - NORMAL ONLY THE PROXIMAL MOST SEGMENT OF RIGHT INTERNAL ILIAC VEIN IS VISUALSED
CT RENAL ANGIO REPORT : BILATERAL SINGLE RENAL ARTERIES ARE NORMAL IN CALIBRE AT ORIGIN , PROXIMAL SEGMENTS : B/L ILIAC VESSELS - NORMAL SINGLE RENAL ARTERIES ARE NOTED , WHICH ARE NORMAL IN CALIBRE AT ORIGIN ( LENGTH OF RIGHT RENAL ARTERY -2.9CMS LENGTH OF LEFT RENAL ARTERY -2.7 CMS THICKNESS OF RIGHT RENAL ARTERY- 4.4MM THICKNESS OF LEFT RENAL ARTERY-5 MM AT ORIGIN CALIBER OF BILATERAL DISTAL MAIN RENAL ARTERIES AND INTRARENAlARTERIEARE REDUCED IN SIZE AND SHOWS NORMAL CONTRAST OPACIFICATION ECENTERIC NON STENOTIC CALCIFIED PLAQUES SEEN AT ORIGINS OF BILATERAL MAIN RENAL ARTERIES BILATERAL SMALL FOR SIZE SHRUNKEN KIDNEYS WITH NO OBVIOUS CONTRAST EXCRETION NOTED IN THE DELAYED UROGRAM STUDY
PULMONARY FUNCTION TESTS SPIROMETRY WITHIN NORMAL LIMITS AS (FEV1/FVC)%>95AND FVC %PRED>80
HLA TYPING DONE
LYMPHOCYTE CROSSMATCH TEST CROSS MATCHING OF PATIENTS SERUM - NEGATIVE WITH DONORS LYMPHOCYTE { % OF LYSED CELLS -3% SCORE }
ULTRASOUND ABDOMEN : B/L SMALLKIDNEY WITH GRADE 3 RENAL PARENCHYMAL DISEASE CHANGES NO PLEURAL
02-03-21 :
E COLI >10*4 CFU / ML OF URINE ISOLATED SENSITIVE TO NORFLOXACIN / NITROFURANTOIN/ COTRIMOXAZOLE/FOSFOMYCIN/ AMIKACIN /OFLOXACIN / PIPPERACILIN/ TAZOBACTUM /MEROPENEM
02-03-21: THROAT SWAB FOR C/S: KLEBSIELLA SPECIES GROWN SENSITIVE TO COTRIMOXAZOLE /CIPROFLOXACIN/ AMIKACIN/ CEFEPIME/ PIPERACILIN / TAZOBACTUM/ MEROPENEM
URINE FOR C/S 5-3-21: E COLI 2X10*3 CFU/MLOF URINE ISOLATED SENSITIVE TO NORFLOXACIN / NITROFURANTOIN/ COTRIMOXAZOLE/FOSFOMYCIN/ AMIKACIN /OFLOXACIN / PIPPERACILIN/ TAZOBACTUM /MEROPENEM
3-3-21: BLOOD C/S : SKIN COMMENSALS GROWN
03-3-21 : SPUTUM FOR C/S : KLEBSIELLA SPECIES GROWN SENSITIVE TO COTRIMOXAZOLE /CIPROFLOXACIN/ AMIKACIN/ CEFEPIME/ PIPERACILIN / TAZOBACTUM/ MEROPENEM
09-4-21 2D ECHO : MILD TR + WITH PAH TRIVIAL AR + NO MR NO RWMA NO AS/MS GOOD LV SYSTOLIC FUNCTION NO DIASTOLIC FUNCTION , EF- 62% NO PE BLOOD FOR C/S : NO GROWTH SEEN URNE FOR C/S :
14-4-21 URINE FOR C/S : NO PUS CELLS AND NO GROWTH
10-4-21 ;NASAL SWAB FOR C/S : NO PATHOGENIC ORGAMNISM ISOLATED
ON 16-5-21 , LIVE DONOR TRANSPLANT DONE
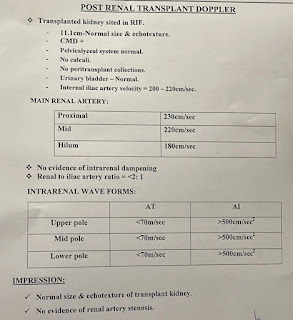
POST TRANSPLANTATION RENAL DOPPLER :
IVC DIAMETER @ HIGHER LRVRL - 18 MM TRANSPLANT RENAL SIZE 10.5 CM ECHOGENECITY AND CMD - NORMAL NO HYDRONEPHROSIS NO COLLECTION INTRARENAL RI :UPPER POLE -0.4 MID POLE -0.4 LOWER POLE -O.4 NO TARDUS NO PARVUS WAVE FORMS GLOBAL PERFUSION IS ADEQUATE MAIN RENAL ARTERY @ HILUM - TURBELENT FLOW WITH PSY 150-200 CM/SEC MAIN RENALARTERY POST PROXIMAL TO HILUM PSY 180-190 CM/SEC NO OBVIOUS FEATURES OF RENAL ARTERY STENOSIS.
TREATMENT GIVEN & OPERATION NOTES :
PRE OPERATIVELY COVID 2019 1ST AND 2ND DOSE GIVEN AT 25-03-21 HBV & PCV BOOSTER DOSE GIVEN HIB VACCINE GIVEN
12-4-21 HLA TYPING DONE LYMPHOCYTE CROSSMATCH IN FASTING MHD DONE
15-4-21. LAST DIALYSIS DONE
MYCOFENOLATE MOFETIL 500 MG @ 8:00 PM
TAXIM 1 GM @ NIGHT AFTER TEST DOSE
NIGHT ANTIHYPERTENSIVES
OT DAY
16-4-21 3 AM ATG 25 MG ( 4 HRS BEFORE SURGERY )STAT + INJ HYDROCORT 100 MG STAT +INJ PCM 1 GM STAT + INJ AVIL STAT INJ MAGNEX FORTE 1.5 GM 1/2 HR BEFORE SURGERY INJ CLEXANE 20 MG
OPERATION NOTES
SURGERY : LIVE DONOR RENAL TRANSPLANTATION - RECIPIENT DONE Renal artery to internal iliac artery ( end to end anastomosis) Renal vein to external iliac vein ( end to side anastomosis) Ureter to bladder (modified lich gregoir anastomosis )
VITAL CHART - POST OP PERIOD.

POST OP BP CHARTING
POST OP ABG TRENDS
MYCOFENOLATE 750 MG @ 8;00 PM
POD 1-2- INTIAL2 DAYS OUTPUT MAINTAINED AROUND 4-5 LITRES
POD-2
TAB . TACROLIMUS 3MG-0-2MG STARTED
INJ LASIX 20 MG , 2 DOSES WAS GIVEN THEN URINE OUTPUT INCREASED TO 8 LITRES PER DAY
POST OP BP MANAGEMENT
POD 2-20 -
Antihypertensive optimisation on POD 4
POST OP PERIOD UNEVENTFUL FOLEYS REMOVED ON POD-5 ON POD-6 ABDOMINAL DRAIN WAS REMOVED POD 12 SUTURE REMOVAL DONE
ON POD 21 - DJ STENT REMOVAL DONE UNDER LA
PATIENT WAS DISCHARGED ON POD 26.
POST OPERATIVE TREATMENT :
PROPPED UP POSITION
ALLOW ORALSIPS OF WATER INTERMITTENTLY
IVF NS, RL,DNS @ URINE OUTPUT +30 ML /HR
INJ SOLUMEDROL IV 500 MG MORNING 250 MG EVENINGON POD -0 FOLLOWED BY 250 MG BD THEN SLOWLY TAPPERED ON POD-3
TAB MYCOFENOLATE MEFOTIL 750 MG BD
INJ . MAGNEX FORTE 1.5 GM IV BD
INJ PAN 40 MG IV BD
INJ NEOMOL 1G IV TID
INJ CLEXANE 20 MG SC @ 3:00 PM
TAB . ARKAMINE 0.2 MG TID
CAP.NIFIDIPINE 5 MG SUBLINGUAL IF BP SHOOTS >220/110 MM HG
TAB AMLONG 10 MG BD
OINTMENT THROMBOPHOBE FOR L/A
CANDID MOUTH PAINT
NEB WITH BUDECORT AND MUCOMIST 8TH HRLY
CHEST PHYSIOTHERAPY 8TH HRLY
INJ HEPLOCKIN IV LINES SOS
TAB . TACROLIMUS 3MG- 0 -2MG ADDED FROM POD 2
TAB WYSOLONE 20 MG BD ADDED FROM DAY 5 AND TAPPERED SLOWLY TO 15 MG -0- 10 MG AND THEN FROM 15-05 -21 TO 10MG-0-10 MG
ADVICE ON DISCHARGE
NORMAL DIET
1. ORAL FLUIDS UPTO 3-4 LITRS / DAY
2.TAB PAN 40 MG DAY TWO TIMES A DAY (BEFORE FOOD )
3.TAB MYCOFENOLATE MOFETIL 750 MG TWO TIMES A DAY
4.TAB TACROLIMUS TWO TIMES A DAY - 3 MG @ 7 A.M &2 MG @ 7 P.M
5.TAB VALGANCYCLOVIR 450 MG ONCE A DAY @ 8: 00 PM
6.TAB SEPTRAN - DS (160/800) MG 1/2TAB ONCE A DAY @ 8: 00 PM
7.TAB WYSOLONE TWO TIMES A DAY AFTER FOOD -10MG @ 8 A.M &10 MG @ 8 P.M
8.TAB .ARKAMINE 0.2 MG FOUR TIMES ADAY 6 AM- 12AM - 6 PM - 12 AM
9.TAB AMLONG 20 MG @ 8 A.M &20 MG @ 8 P.M
10.TAB MET XL 50 MG @ 8 A.M &500 MG @ 8 P.M
11.TAB B COMPLEX OD @ 2 PM
12.INCENTIVE SPIROMETRY
13 SYP . AT 15 ML SOS
14 .CANDID MOUTH PAINT
15 .INHALATION WITH BUDECORT INHALER BD
Follow Up FOLLOW UP AFTER 2 MONTHS IN KIMS NARKETPALLY
Since then Patient RFT values are monitored monthly and patient is on teleconsultation twice monthly.
In December 2021 patient came for follow up then RFT was normal & transplant kidney Doppler was normal.
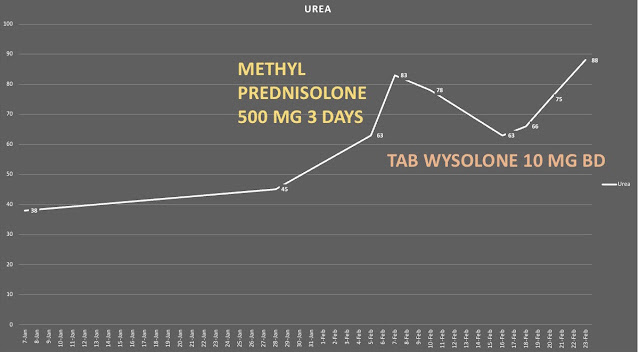
On routine check up in February patient renal profile shows Sr.Cr 1.8, urea 45. Advised to come to Narketpally for follow up & evaluation for rejection. Patient repeated RFT again after 1 week then Sr.Cr 3.2 & urea 65.
CURRENT ADMISSION FEB 2022 - CHRONIC CELLULAR REJECTION.
Then patient came to KIMS NKP on 16th February and evaluated for deranged RFT. All routine investigation are normal except for renal profile.
Patient missed the steroid doses as there was some discrepancy in online vs offline consultation.
Transplant kidney Doppler was done showing :
Significantly increased peak historic velocity is origin of right transplant Main renal artery at anastomotic site with iliac artery
the intra renal arteries at all poles show mild reduced flow velocity at early features of Tardus Parvus flow pattern.
The ratio flow velocities of transplant Main renal artery to right external iliac artery is 3.7
Above all features suggestive of likely possibility of moderate stenosis at right transplant renal artery at anastomotic site.
Mild increased parenchyma changes at transplant kidney
Advised CT renal angio correlation and follow-up
In view of cellular rejection high dose methyl prednisone started @ 500mg twice daily followed by Tab. WYSOLONE 10mg BD. Following which creatinine trends decreased.
In view of increased hemoglobin value Tab. ENALAPRIL 2.5 mg BD started.
After discussion among Treating urology, nephrology and internal medicine team we planned for DTPA scan for Transplant kidney and CT renal angiogram is postponed in view of decreasing trends of creatinine.
Tc99DTPA scan reveals normal perfusion & normal function in the transplanted kidney with moderately prolonged cortical transit - possibly due to Nephrotoxic drugs.
Tc99m DTPA scan has been done. After discussing the case On telemedicine with Dr. Xxx (consultant) who signed the report he gave this opinion.
1. Satisfactory perfusion of transplanted kidney
2. Satisfactory function of transplated kidney ( good gfr)
3. Unlikely Renal artery stenosis but to rule out completely, Captopril study is needed but it may cause transient renal shutdown and anuria atleast 24-48h
4. Structyand functional aspects of kidney is satisfactory, but due to prolonged cortical Transit the report is given as toxicity of nephrotoxic drugs.
Renal biopsy done on 1st March of the transplanted kidney
Discussion :
1) A Randomized, Multicenter Study of Steroid Avoidance, Early Steroid Withdrawal or Standard Steroid Therapy in Kidney Transplant Recipients
I - Steroids to day 7 (n = 115), or standard steroids (n = 109) with cyclosporine
C - Patients received no steroids (n = 112)
Received no steroids steroids to day 7 (n = 115), or standard steroids (n = 109) with cyclosporine
The primary objective, to demonstrate noninferiority of 12-month GFR in the steroid-free or steroid-withdrawal groups versus standard steroids, was not met in the intent-to-treat population
There were no significant differences in GFR at month 12 between these groups
By month 12, nine patients (2.7%) had died and nine (2.7%) lost their grafts, with no significant differences between groups.
Graft loss or death was significantly higher only in the steroid-free group versus the standard-steroids group
https://onlinelibrary.wiley.com/doi/10.1111/j.1600-6143.2007.02057.x
2) A retrospective cohort study
P - A total of 6070 first kidney transplant recipients who were transplanted between 1990 and
2012 were evaluated and classified according to steroid treatment status throughout follow-up after kidney transplantation
O - In total, 2142 patients were withdrawn from steroids within th.e study period. Median follow-up time was 6.5 years.
Functional graft loss
Overall, 1131 patients in our study cohort lost their graft within the study period.
The rate of graft loss was significantly higher for patients who were withdrawn from steroids within the first 18 months after transplantation compared to steroid maintenance during this time
Our results demonstrate that steroid withdrawal within the first 18 months after transplantation is associated with an increased rate of graft loss compared to steroid maintenance during that time, while mortality is unaffected by steroid withdrawal at any time point after transplantation compared to steroid maintenance
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-016-0772-6
On 6/3/22
Yesterday ( 6/3/22) patient developed 3 episodes of bleeding during defecation as described by the patient first stool followed by a gush of blood.
General surgery opinion was taken : as per there per rectal examination there was no fissures, polyps, hemorrides. How ever proctoscopy was inconclusive due to blood in the feild. Packing was done.
There was significant drop in hemoglobin from 15 to 8 gm/dl.
Planning for colonoscopy and endoscopy.
Endoscopy and colonoscopy done shows no active bleed and incidentally detected polyp in colon.
Colonoscopy
Endoscopy :
Biopsy report awaited...






















Well done Dr. Kulkarni
ReplyDelete