25F post partum with shortness of breath
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient' problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Thanks to : Dr. Keerthi (JR1) Sneha (MBBS 8th sem), Suhitha (intern),
3/11/22
25 year old female, mother of 2 babies resident of Nalgonda with history of consangious marraige presented to us with complaints of worsening Breathlessness and both lower limb swelling since a week.
Problem representation-
25F with Multisystemic Inflammatory syndrome with background of Eclampsia and preterm delivery
Reviewed patient today
Complaints of sob yesterday night.
Excess daytime drowsiness
Fever decreased
No seizures
O/E: Pt is c/c/c
Bp- 130 /70 mm hg
PR- 88 bpm
RR-30 can
Spo2- 96% on 4L o2
CVS- S1 S2+ with pan systolic murmur @aortic area
RS- BAE+/Mild IAA crepts
B/L pupils NSRL
Labs-( acute glomerular injury.(increased urea/increased creatinine / 24hp=>300mg/dl)
Thrombocytopenia, elevated liver enzymes
HELLP - subsiding
Hepatosplenomegaly with mild ascites
Deranged coagulation profile
Reversible heart failure with ? Pulmonary artery hypertension with minimal pericardial effusion
MRI-F/S/O PRES
USG-Grade 1 RPD
ECG- S1Q3T3 with sinus tachycardia.
Peripheral smear showing presence of schistocytes.
Bleeding from central line site probably due to derranged coagulation profile.
CXR at Admission
Infections - Sepsis with MODS
Autoimmune - SLE, APLA, MAHA
Toxins - HUS
Differential diagnosis
1. ? AKI (intrensic) secondary to Autoimmune disorders-? SLE/? APLA
2.MODS with DIC (Non infective > Infective)
Rx
INJ. PIPTAZ 2.25 MG IV/BD
1.INJ.LASIX 80 MG -X- 40 MG IV/BD
2.TAB.NICARDIA RETARD 20 MG/PO/TID
3.TAB.MET XL 50 MG/PO/BD
4.TAB.LEVIPIL 500 MG/PO/BD
5.TAB.ECOSPIRIN 75MG/PO/OD
6. TAB. DOLO 650MG PO/BD.
7.Fluid and salt restriction
8.VITALS MONITORING 4th hourly
On 7/11/22
On 9/11/22
On 10/11/22
Update on 11/11/22
25 year old female with background history of , multiorgan dysfunction syndrome ( acute glomerulonephritis, acute hepatitis (resolved) , hemolytic anemia with thrombocytopenia) presented with worsening shortness of breath and fever associated with dry cough(occasional)
1. Patient is breathless with rr 30 cpm
2. Cough with blood tinged sputum (resolving)
3. Fever spikes ( resolving)
4. Last session of HD yesterday
Course in the hospital:
With the background history of eclampsia, HELLP syndrome, acute cardiogenic pulmonary edema. Patient was dialysed under blood transfusion (PRBCs blood) coverage and evaluated for the cause of multiple system organ dysfunction (AGN,AILI,hemolytic anemia with thrombocytopenia)
Infections and autoimmune etiologies were considered.
Patient was started on antibiotics, antihypertensives with preload ? agents , continued anti epileptics .
OBG opinion was taken in view of eclampsia and HELLP syndrome. Advice followed.
In hospital patient developed severe cough associated with blood tinged sputum. Ecospirin was witholded
Heparin free dialysis was since admission in view of thrombocytopenia
Tab HYDRALAZINE was added to control the blood pressure. Initial blood cultures at admission was negative for organisms. ANA profile with P & C-ANcA and C4 are within normal limits
On antibiotics patient was planned for renal biopsy but due to pulmonary edema and fever procedure is postponed.
Repeated blood culture shows klebsiella sensitive to meropenem
Urine culture shows klebsiella sensitive only to fosfomycin( considered as colonies) with no symptoms of UTI
Sputum culture sensitivity negative
After adding meropenem patient’s fever spikes decreased
X ray showing worsening pulmonary edema ( non cardiogenic> cardiogenic)
Pulmonologist opinion was taken in view of ? Non cardiogenic pulmonary edema and advise was followed.Inj clindamycin was added in view of ? Pneumonia
Cardiologist opinion was taken in view of cardiogenic pulmonary edema. Patient was started on NIV intermittently. ABG Showing hypoxia
Pt is c/c/c
Bp- 150/100 mmhg
Pr - 110 bpm
Rr- 30 cpm
Cvs - s1s2 + / jvp raised ( decreased)
S3 gallop and pansystolic murmur (subsided)
RS- BAE + , B/L IAA, IMA crepts
Cns - no fnd
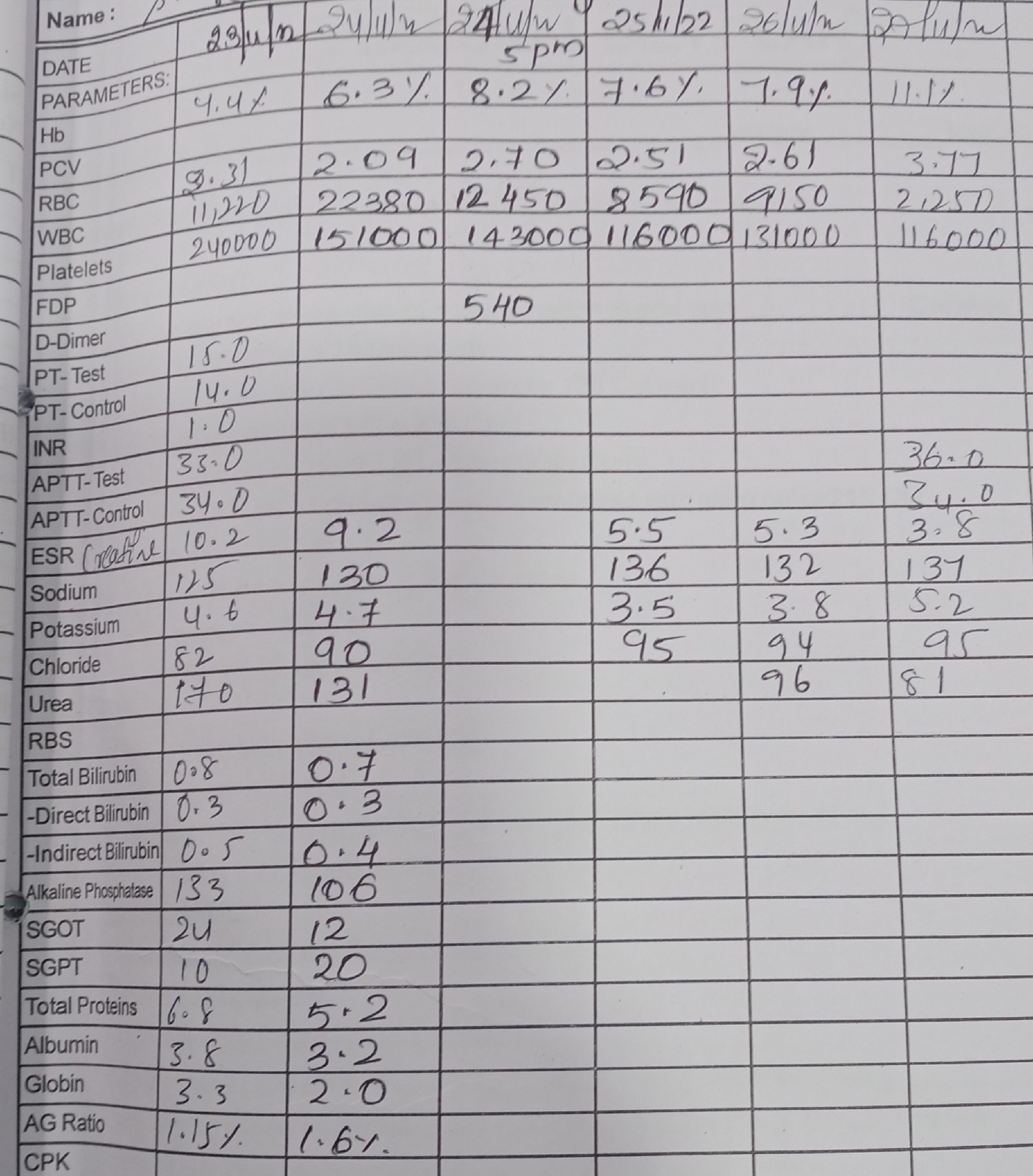
Labs-
1. Worsening AKI and pulmonary edema
2. Thrombocytopenia ( resolved)
3. Liver enzymes normal (8/11)
4. Hemolytic anemia (subsided)
5. Coagulation profile - improving
6. Fair LV systolic function with minimal pericardial effusion
7. Gr- I rd changes and hepatosplenomegly
8. ECG- sinus tachycardia with ST elevation @ II, III
Diagnosis- acute kidney injury secondary to gram negative bacterial sepsis( klebsiella) with ? Hospital acquired pneumonia
S/P hemodialysis on NIV - PC
K/c/o eclampsia with HELLP syndrome ( resolved)
24H PINK FROTHY SPUTUM
BP charting
SBP
DBP
Adv-
NIV - ventilation
Optimisation of antihypertensives
Continue antibiotics.
Continue Hemodialysis
BP,PR,RR,TEMP every fourth hourly
Strict I/O monitoring
Plan for renal biopsy tomorrow if patient is hemodynamically stable
12/11/22
Patient developed SOB at morning 7am. Took her antihypertensives as per schedule. Lung auscultation is clear. BP 150/100mmhg, PR 120, temp 103F. Planned biopsy was postponed.
Chest xray :
ECG :
In view of history, clinical examination, laboratory evaluation, clinical huntch of HUS/TTP was made and Nephrology team decided to refer the case to higher center for further evaluation ( Biopsy) and management ( plasmapharesis ).
Patient attenders took her to home in misconception of black magic Taboo, where she was apparently same for 6-7 days. Then she developed worsening shortness of breath with decreased urine output.she was admitted at nearest corporate center.
At admission patient had breathlessness at rest with Generalised body swelling and decreased urine output. Following evaluation was done.
Femoral dialysis catheter is removed and new IJV catheter placed. Arterial line was placed to monitor BP. In view of respiratory distress patinet was intubated and kept on Mechanical ventilation. Dialysis was done under PRBC transfusion coverage.
BLOOD WORK UP
URINE ANALYSIS
PROCALCITONIN
D-dimer
2d Echo
HRCT CHEST
Treatment
In a close interview with patients husband, he broke down into tears that his new born daughter is in Apex government pediatric center of the state and no one is there with her. She is under the care of Hospital and police staff since patient was discharged from our hospital.
He sold his flat and land to bear the cost of medical bills. Till now he spent around 12-13 lakhs in corporate hospitals ( 1-1.5 lakhs in our center which was covered under State health scheme for dialysis and Respiratory failure ).
Patient is in Mechanical Ventilator planning for tracheostomy and renal biopsy.
29/11/22 :
In view of difficulty in weaning off from ventilator, tracheostomy was done today.
30/11/22
Patient still on Mechanical Ventilator
Repeat HRCT chest was done. Showing F/s/o pulmonary edema.
1/12/22
[12/2, 8:22 AM]: Yesterday's x ray...she didn't maintain even saturation with 100 FiO2...
[12/2, 8:23 AM]: Went into hypotension, started with dual inotropes
[12/2, 8:24 AM] : Poor prognosis explained ...so patient attendants took her home on LAMA
At 11.00pm she expired.




































Comments
Post a Comment